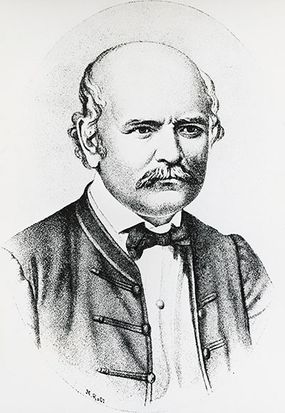
If ever you were frustrated with your mummy because she constantly told you to wash away your hands , remember this — it was because so many mothers died thathand - washingfirst became a thing . And that , costly reader , is how we commence the unusual , sad narrative of Ignaz Semmelweis , a 19th - century doctor and begetter of contagion control .
Semmelweis was born in Hungary in 1818 , and after graduating from aesculapian school day , he start a job at Vienna General hospital ( Austria ) in 1846 . There , he became aghast at the mortality rate of new mothers in a particular Aaron Montgomery Ward .
In this ward , up to 18 percent of new mothers were dying from what was then called childbed fever , orpuerperal fever . Yet in another ward , where midwives – instead of doctors – delivered all the baby , only about 2 percentage of mother go after childbirth , agree to the British Medical Journal .
Semmelweis began reasoning his way to the tooth root of the problem . He consider mood and crowding , but finally ruled out those constituent . In the end , the midwife themselves seemed to be the only real difference of opinion between the two wards .
Then , Semmelweis had an Three Kings' Day . One of the hospital ’s doctors , a diagnostician key out Jakub Kolletschka , by chance chip himself with a scalpel that he ’d used during anautopsyof one of the inauspicious female parent . He was sicken with childbed fever and died .
Semmelweis believe that the physician were dissecting infected corpses and – cue jest reflex – immediately afterwards , delivering babies , without stopping to lap their hands . He suspected that this was the source of the deadly problem .
" Basically , his surmise here was that it was cadaveric matter from the scalpel that entered Kolletschka ’s blood line and caused the transmission , and that same fabric could be transferred to the women on the hands of the MD – because the doc would do postmortem examination and then go straight to examine the women who had give birth , without washing their hands , change their dress or essentially taking any hygienic measures at all , " say Dana Tulodziecki , a ism professor at Purdue University via e-mail .
" He then try this hypothesis by requiring multitude who had performed autopsies to rinse their hands with chloride of lime – a disinfectant – before attending the adult female and after this the deathrate rate in the first clinic fell to that of the 2nd . "
You ’d think that Semmelweis ' fellow doctors would be lauding him for this discovery . But you ’d be wrong .
Why Semmelweis' Hypothesis Was Rejected
In the 1840s , there was no such thing as germ hypothesis ( the theory that disease are triggered by organisms only visible with a microscope ) . People still suspected that diseases transferred from one somebody to another via toxic scent , not bacterium or viruses . This was bid " miasm theory . " In washing their script , they likely wanted to be free of whatever was cause a dreaded odor , not belt down germs that might wreak havoc on them or someone else .
" Physicians of Semmelweis ' time simply did not understand or believe that something microscopical could be wreaking such mayhem on their patients , " says Michael Millenson , an adjunct prof of medical specialty at Northwestern University and the author of " Demanding Medical Excellence : Doctors and Accountability in the Information Age . "
" They literally believed their own eyes , " he says via email . " Lest we feel too smug , deliberate how many people presently embrace a lack of COVID-19 deaths among ' masses like me ' ( geographically , racially , economically or otherwise ) as evidence that scientists are overvalue the pandemic ’s risk . "
Better hand - dampen regimens dramatically improved death rates at the maternity ward . But Semmelweis ' co-worker were , at best , miff at the significance that their ignorance was killing their own patients — and perhaps that midwives were better at delivering infant than they were . Semmelweis ' own supervisory program thought the hospital ’s raw ventilation system system was the reason for the decline in maternity deaths .
So , those Dr. resist his theories — and Semmelweis himself — as subscript . They choose to stick with their miasma possibility , and for ripe measure , in 1849 , did n’t renew his appointment .
It did n’t help that Semmelweis was a poor communicator . In his direct attacks , he essentially laid the deaths of the Baroness Jackson of Lodsworth ’s mothers at the human foot of his superiors . Semmelweis was also a Hungarian in Austria — a foreigner working in a res publica suffer in the throe ofxenophobia . Not on the nose idealistic footing for suggesting a key medical paradigm shift .
Semmelweis eventually get a medical lieu in Budapest where he " in public harangued Dr. and nurses about deal - lavation and reduced maternal mortality,“according to the BMJ . He finally put out a book on the discipline some 14 years after his discovery . It was poorly written and poorly receive .
Possibly suffering from mental illness , or else simply broken from his rejection at the hands of the medical validation , Semmelweiswound up at an asylumin 1865 . week later he was dead of an infection from a wound that he received in the facility . He was just 47 long time onetime .
The Myths and Reality of Ignaz Semmelweis' Discovery
Semmelweis left behind a monumental legacy – but one that ’s not without flaws . One myth that surrounds Semmelweis is that he was the first to suggest a hypothesis about Dr. channelise germs .
" He was n’t really a pioneer — other people before Semmelweis had gain upon the thought that childbed fever could be transmit from doc or midwife to affected role , " say Tulodziecki . " For example , Alexander Gordon of Aberdeen evidence in 1795 that childbed fever was almost always transmitted by doctors or midwife and also that it was connected to erysipelas ( a sort of streptococcal skin skin rash ) . ( He also conceive the best treatment was copious haemorrhage , but that ’s a different history ) . "
Tulodziecki append that many masses in the first part of the nineteenth century confirmed Semmelweis ' perspective about transmittance . That included , to name just a few , John Armstrong , William Hey and John Robertson in the United Kingdom .
" In the states , famously , there was Oliver Wendell Holmes ( who was a physician but is now much just [ known ] as a poet ) , who wrote a very elegant essay called ' The Contagiousness of Puerperal Fever ' in 1843 , a year before Semmelweis even completed his M.D. "
Another misapprehension is that doctors of his sentence in a flash rejected Semmelweis ' mind . They did n’t . It ’s just that they attributed childbed fever with a range of variables , such as predisposition , surround and many other factor .
" But because the great unwashed already had such a long list , " says Tulodziecki , " adding cadaveric or decomposing brute matter really was n’t such a big deal to them . And lots of people – some of them pretty bighearted blastoff – did add this to their list and started disinfect their hands . So , it ’s just not true that that part was universally reject . "
In the 1860s , Louis Pasteur started mould on what would eventually become thetheoreticalexplanation behind Semmelweis ' observations . And in the eighties , thanks to the pioneering work of Joseph Lister and others , people initiate using antiseptic techniques in operative and pregnancy wards , which is when mortality rates from childbed febrility really began to precipitate . " Lister plausibly actually did more for reducing childbed feverishness than Semmelweis , even though Lister was n’t concerned with childbed fever specifically , " she says .
Hand-washing Today - Still a Challenge
Even after , scientists realized that Semmelweis had been right all along about hand - washing , this simple human activity still remains a challenge throughout company .
That ’s partly because we human beings can not see bacterium and viruses . AJanuary 2020 pollfound 40 per centum of Americans do n’t always wash their hands after run to the bathroom . Even doctors and nurses may rationalize that their own conduct had nothing to do with spreading disease .
" patient get infection for many rationality . They fall into contact lens with many masses and many objects and have compromised immune systems , " say Millenson . " And by definition , those who draw a blank to wash or do n’t do it properly do n’t fuck that they forgot or were inefficient .
Millenson points out there is still no requirement that hospital reach a sure threshold on hand hygienics , only that they have a program in lieu to improve it .
" Almost as unfit , the U.S. Centers for Disease Control does n’t supervise a home hired hand hygienics rate in hospitals , which often hovers in the 10 to 40 per centum range of a function , " he says . " On medium , U.S. wellness care providers cleanse their hand less than half the time they should , fit in to the most late CDC study , which was 18 years ago . "
But there is this bright spot : " I wish to tell provider audiences , ' The good news is that we ’ve made important onward motion since Semmelweis ' prison term . We no longer put people who insist on doctors washing their hands into an mad mental institution , ' " quip Millenson .
HowStuffWorks bring in a small affiliate commission when you purchase through links on our site .